- Review
- Open access
- Published:
Type 1 diabetes mellitus: retrospect and prospect
Bulletin of the National Research Centre volume 48, Article number: 42 (2024)
Abstract
Background
Type 1 diabetes (T1D) is an autoimmune disease leading to destruction of insulin-producing pancreatic beta cells. Both genetic and environmental factors contribute to pathogenesis. The incidence of T1D is increasing worldwide, with significant geographic and ethnic variations. Patients present with symptoms of hyperglycemia and diabetes complications.
Main body
In T1D, autoreactive T cells and autoantibodies destroy beta cells, causing insulin deficiency. Exogenous insulin therapy is essential but cannot replicate normal physiology. Management requires intensive lifestyle education on diet, exercise, glucose monitoring and avoiding complications, in addition to insulin. Novel therapies like immunotherapy, cell transplantation, artificial pancreas devices and AI algorithms aim to improve care. Strategies for reversing T1D involve combination immunotherapies to block autoimmunity and regenerate beta cells via stem cells or xenotransplantation.
Conclusion
While type 1 diabetes remains challenging, ongoing research provides hope. Elucidating individualized disease mechanisms and translating findings into precision prevention and treatment approaches are critical to improving long-term outcomes. Innovative and multi-targeted therapies may fundamentally change the trajectory of T1D.
Background
Type 1 diabetes (T1D) is an autoimmune disease characterized by the T cell-mediated destruction of insulin-producing pancreatic beta cells, resulting in insufficient insulin production and hyperglycemia. T1D represents 5–10% of all diagnosed diabetes cases and most often develops in children and adolescents, but can occur at any age (Popoviciu et al. 2023). There are significant ethnic differences in T1D incidence, with much higher rates reported in populations of European descent compared to other ethnicities. In the USA, the incidence rate was highest among non-Hispanic whites (24.8/100,000 per year) compared to Hispanic (17.2/100,000), African-American (11.3/100,000), and Asian American populations (8.5/100,000). The reasons for wide geographic and ethnic variation are not fully understood, but are likely related to differences in genetic susceptibility and environmental exposures. The development of T1D is influenced by both genetic and non-genetic factors. There is a strong genetic component, with the HLA region accounting for 30–50% of genetic susceptibility. Specific HLA haplotypes such as DR3-DQ2 and DR4-DQ8 are linked to higher risk. However, only around 10% of individuals with high-risk HLA genotypes develop T1D, highlighting the importance of environmental factors (Ogrotis and Koufakis 2023). Patients with type 1 diabetes have increased risk of stroke, likely due to hyperglycemia-induced vascular dysfunction (Liu et al. 2021). T1D promotes non-alcoholic fatty liver disease and fibrosis through insulin deficiency, lipolysis, and metabolic dysregulation (Addissouky et al. 2021). H. pylori infection may be linked to T1D onset by promoting inflammation and molecular mimicry between H. pylori antigens and islet autoantigens (Addissouky et al. 2023a, 2023b), though more evidence is needed to confirm this association. Several environmental contributors have been identified, including early infant nutrition, viral infections, gut microbiome composition, and vitamin D status. Early exposure to complex foreign proteins like dairy and gluten may stimulate autoimmunity in genetically susceptible infants. Enteroviral infections have been frequently isolated from the pancreas of newly diagnosed T1D patients and may act as triggers of autoimmunity. Dysbiosis of the gut microbiome with reduced diversity has been associated with T1D development. Vitamin D deficiency may also confer increased risk, possibly by modulating immune responses. Psychosocial stress and low socioeconomic status have been less consistently linked to T1D (Corsello et al. 2023). On a molecular level, the pathogenesis involves both cellular and humoral autoimmune destruction of beta cells. CD4+ and CD8+ T cells directly attack beta cells displaying autoantigen epitopes like insulin, GAD65, IA-2, and ZnT8. Autoantibodies against these antigens are present years before clinical diagnosis and are important diagnostic markers. Pro-inflammatory cytokines like IL-1β, IFNγ, and TNFα secreted by infiltrating immune cells create a toxic microenvironment within the islets damaging beta cells (Francesca et al. 2022). Genetic susceptibility along with environmental encounters leads to breakdown of immunological tolerance and activation of autoreactive T and B cells. Defects in regulatory T cells that suppress autoimmunity and altered intestinal barrier function permitting microbial translocation may be contributory. Ultimately, there is a prolonged subclinical period of insulitis where a majority of beta cell mass is destroyed before onset of symptomatic hyperglycemia. Elucidating these molecular events may allow for development of antigen-specific immunotherapies to intercept the pathogenesis of T1D (Holborough-Kerkvliet et al. 2023).
Global epidemiology of type 1 diabetes
Type 1 diabetes (T1D) is an autoimmune disease characterized by the destruction of insulin-producing beta cells in the pancreas. Recent studies have provided important insights into the global epidemiology of T1D, helping to characterize patterns in incidence, prevalence, mortality, and outcomes. According to the T1D Index, the first comprehensive effort to estimate the global burden of T1D using a Markov model, there were an estimated 8.4 million prevalent T1D cases worldwide in 2021, with prevalence rates varying widely between countries from 1.5 to 534 cases per 100,000 populations (Ogle et al. 2023). Incidence of T1D also demonstrated geographical heterogeneity, ranging from 0.02 to over 50 cases per 100,000 children under 15 years of age. While T1D has traditionally been viewed as a disease of children and adolescents, the T1D Index findings highlighted that adult-onset T1D accounts for the majority of prevalent cases globally. However, epidemiological data remain limited for adult T1D compared to pediatric populations. Accurately determining incidence and prevalence is further challenged by issues such as misclassification between T1D and type 2 diabetes (T2D) in adults and heterogeneity in T1D phenotypes (Ogle et al. 2023; Ogrotis et al. 2023). National studies have helped address gaps, such as research in Iran finding age-standardized incidence rates increased in both sexes from 1990 to 2019 across different provinces (Bandarian et al. 2023).
A meta-analysis of 55 countries from 2000 to 2022 reported significant variations in T1D incidence among children and adolescents, with the highest rates found in Nordic countries and Sardinia (Hormazábal-Aguayo et al. 2024). Moreover, studies have shown evolving incidence trends over time that differ between populations and world regions, underscoring the need for ongoing surveillance (Ogle et al. 2023; Berthon et al. 2023). The T1D Index also estimated that in 2021, approximately 35,000 deaths in those under 25 years of age were attributed to a lack of T1D diagnosis. Such “deaths from non-diagnosis” predominantly impacted low- and middle-income countries in Sub-Saharan Africa and South Asia. In terms of outcomes, the T1D Index model predicted considerable disparities globally in health-adjusted life years based on estimated differences in access to diabetes care (Ogle et al. 2023). Other population-based studies have since also reported variability in life expectancy and mortality rates associated with T1D depending on timeframe, region, and quality of management (Arffman et al. 2023). Taken together, these findings highlight the importance of strengthening T1D epidemiology surveillance efforts internationally, as recognized by expert groups, in order to most effectively guide public health strategies and resource allocation to improve diagnosis rates and patient outcomes on a global scale (Beran et al. 2023).
Pathogenesis of type 1 diabetes
The pathogenesis of type 1 diabetes (T1D) is mediated by an autoimmune attack targeted against the insulin-producing pancreatic beta cells. Both autoreactive T cells and autoantibodies contribute to selective destruction of beta cells, causing insulin deficiency and hyperglycemia. The pathogenesis is complex, involving interactions between genetic and environmental factors that trigger loss of immunological tolerance.
Destruction of beta cells
Progressive loss of pancreatic beta cell mass and function is the central feature in T1D pathogenesis. The process begins months to years before clinical diagnosis, as evidenced by detection of multiple autoantibodies during pre-symptomatic stages. Histological examination of pancreata from T1D patients reveals insulitis, characterized by infiltration of immune cells including T lymphocytes, B lymphocytes, macrophages, and dendritic cells into the islets. Cytokines secreted by these inflammatory cells induce beta cell apoptosis. Near complete beta cell destruction, around 80–95%, occurs by the time hyperglycemia is apparent. Both CD4+ and CD8+ T cells directly attack beta cells displaying processed autoantigen peptides via the HLA class I and II pathways. The beta cell antigens targeted include insulin, glutamic acid decarboxylase 65 (GAD65), insulinoma-associated antigen 2 (IA-2), and zinc transporter 8 (ZnT8). Environmental triggers like viral infections are thought to initially damage beta cells, releasing autoantigens that activate autoreactive T cells. These cells proliferate and recruit additional immune cells to maintain insulitis. Ongoing beta cell apoptosis exceeds any potential for residual beta cell regeneration, until few functional beta cells remain. The pathogenesis of T1D involves both cellular and humoral-mediated autoimmune destruction of pancreatic beta cells. Autoreactive CD4+ and CD8+ T cells infiltrate the islets, releasing inflammatory cytokines and directly attacking beta cells. B cells produce autoantibodies that form immune complexes activating complement. Macrophages and dendritic cells also contribute to insulitis. This multi-pronged assault overwhelms beta cell capacity for regeneration, leading to insufficient insulin secretion (Thompson et al. 2023).
Loss of insulin secretion
The autoimmune destruction of beta cells leads to loss of insulin production and secretion, resulting in impaired glucose homeostasis. Normal beta cells have a remarkable capacity to upregulate or downregulate insulin secretion in response to blood glucose levels. In T1D, this ability to tightly regulate insulin release is damaged early in pathogenesis due to beta cell stresses that disrupt secretory function. Pro-inflammatory cytokines like IL-1β, TNF-α, and IFN-γ secreted by infiltrating immune cells in insulitic islets are toxic to beta cells. They perturb cellular signaling pathways controlling glucose-stimulated insulin secretion. Beta cells initially compensate by increasing insulin output per cell and expanding beta cell mass. But eventually secretory function cannot offset the degree of beta cell death, leading to insufficient basal and post-prandial insulin secretion. The resulting insulin deficiency prevents regulation of hepatic glucose production and peripheral glucose uptake, causing hyperglycemia and classical diabetes symptoms (Sun et al. 2023).
Role of T Cells
CD4+ and CD8+ T cells are major players in the autoimmune attack against beta cells. CD4+ T helper cells recognize beta cell peptides presented by HLA class II molecules. They differentiate into inflammatory Th1 and Th17 subsets in the islet infiltrate, secreting cytokines like IFN-γ, TNF-α, and IL-17 that amplify local inflammation and recruit additional immune cells. Th1 and Th17 cells also provide help to B cells, supporting autoantibody production. CD8+ cytotoxic T cells directly induce beta cell apoptosis upon engaging their cognate autoantigen peptides on HLA class I. Their cytotoxic effects are mediated through release of granzymes, perforin, and pro-apoptotic cytokines. Regulatory T cells that normally suppress autoimmune responses are unable to control the expansion of pathogenic T cells in T1D. Manipulating the balance of autoreactive and regulatory T cells is a strategy being explored for immunotherapy. In addition to conventional CD4+ and CD8+ T cells, other T cell subsets may contribute to beta cell damage. NKT cells recognizing lipid antigens can produce inflammatory cytokines within islets. Gamma-delta (γδ) T cells are expanded in the peripheral blood of T1D patients and may infiltrate islets early in pathogenesis. Their roles require further clarification. Overall, autoreactive T cells at multiple levels mediate the autoimmune attack driving beta cell destruction and dysfunction (Dinić et al. 2022).
Role of autoantibodies
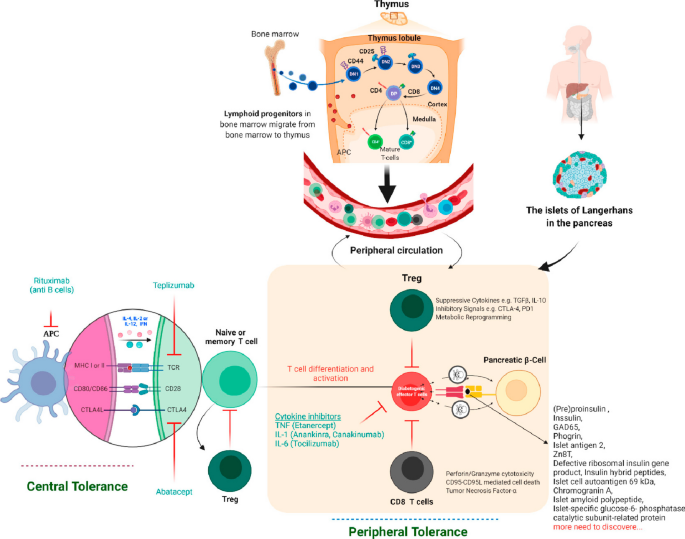
Autoantibodies directed against islet autoantigens are a hallmark of T1D. Their presence indicates ongoing autoimmunity years before clinical diagnosis. Common islet autoantibody specificities include insulin, GAD65, IA-2, and ZnT8. These autoantibodies are produced by B cells that receive T cell help in the islet infiltrate and pancreatic lymph nodes. They are highly sensitive and specific biomarkers, but do not directly induce beta cell death. Rather, autoantibodies contribute to pathogenesis by forming immune complexes that activate complement cascades and inflammatory responses. They also facilitate antigen presentation to autoreactive T cells. Autoantibodies may reflect the degree of T cell-mediated injury and can help predict T1D development in at-risk individuals. Their detection has become important for staging pre-symptomatic disease, stratifying risk in relatives of T1D patients, and recruiting for prevention trials. However, autoantibodies alone are insufficient to cause T1D without collaboration from autoreactive T cells. T lymphocytes originate from bone marrow progenitor cells and mature in the thymus, where central tolerance mechanisms enable them to discriminate between self- and non-self-antigens (negative selection). Regulatory T cells (Tregs) and pathogenic T cells can recognize self- or beta cell antigens, but with differing affinities, which may explain their opposing functions. Mature T cells circulate and may encounter their specific peptide-MHC/HLA complex. In T1D, these T cells target beta cell proteins like insulin, GAD55, and others. If antigen presenting cells display these beta cell peptides on MHC/HLA, T cells activate in lymph nodes, migrate to islets, and destroy beta cells in an antigen-specific manner. Tregs suppress these events as part of peripheral tolerance. If the immune system cannot halt the autoimmune attack on beta cells, insulin deficiency, hyperglycemia, and T1D result. Most signaling occurs locally in lymph nodes and pancreas, evading detection by biomarkers as presented in Fig. 1 (Rathod 2022).
Pathogenesis of T1D autoimmunity (Rathod 2022)
Clinical presentation
The clinical presentation of type 1 diabetes (T1D) reflects the metabolic consequences of insulin deficiency caused by autoimmune beta cell destruction. The symptoms largely relate to hyperglycemia and include polyuria, polydipsia, weight loss, and in severe cases, diabetic ketoacidosis at diagnosis. T1D onset can be abrupt and symptomatic, but a prodrome phase of months to years with mild hyperglycemic symptoms often precedes the classical presentation. Hyperglycemia manifests several weeks to months before diagnosis as beta cell mass and function declines. Glucose excretion in the urine due to renal threshold saturation leads to compensatory polyuria and polydipsia. Nocturia is commonly reported by parents of children with new-onset T1D. Unexplained weight loss may also occur as caloric loss through urination induces catabolism of fat and protein stores. Fatigue, blurred vision, and poor wound healing can result from constant hyperglycemia. In addition to overt diabetes symptoms, the prodrome phase is often characterized by unwellness, irritability, food cravings, and mood changes as glycemic control worsens. In cases where diagnosis is delayed, children and adolescents may present with diabetic ketoacidosis (DKA) as the first manifestation of T1D. Insulin deficiency leads to hyperglycemia and release of glucagon, cortisol, and catecholamines which accelerate lipolysis and ketogenesis. This results in ketone body accumulation causing metabolic acidosis. Patients are typically volume depleted and have Kussmaul respirations trying to blow off carbon dioxide to compensate for acidosis. Abdominal pain, nausea, and vomiting are common along with mental status changes in severe DKA. Cerebral edema is a potentially fatal complication. DKA at diagnosis occurs in 13–80% of pediatric T1D cases, with higher rates in young children. Prompt diagnosis and treatment of hyperglycemia are vital to avoid progression to ketoacidosis. In addition to the classic diabetes symptoms stemming from hyperglycemia, patients with new-onset T1D often have signs and conditions that reflect the underlying autoimmune pathogenesis. There is increased risk for other organ-specific autoimmune disorders, most commonly autoimmune thyroiditis (Hashimoto's thyroiditis). Up to 20% of T1D patients have thyroid autoantibodies, and 2–10% develop clinical hypo- or hyperthyroidism. Celiac disease is another associated autoimmune disorder, affecting 5–10% of individuals with T1D. Symptomatic celiac disease or positive celiac antibodies should prompt screening for T1D-associated autoimmunity. Less common autoimmune conditions like Addison's disease (primary adrenal insufficiency), autoimmune gastritis, vitiligo, and alopecia areata can also co-occur with T1D. Persistent presence of other autoantibodies such as anti-nuclear antibody or rheumatoid factor may signify increased generalized autoimmune tendencies. Patients often have a family history of autoimmunity. Together, the constellation of polyuria, polydipsia, unexplained weight loss, DKA at diagnosis, and concurrent autoimmunity provides clues to the underlying autoimmune etiology of T1D even before diagnostic confirmation (Murdaca et al. 2023).
Treatment and management
Insulin therapy
Type 1 diabetes (T1D) is a chronic condition requiring intensive insulin therapy to manage blood glucose levels and prevent acute and long-term complications. Insulin replacement is essential because patients are unable to produce their own insulin due to autoimmune destruction of pancreatic beta cells. Treatment regimens utilize different types of insulin with varying pharmacokinetic profiles to approximate normal physiologic insulin secretion. Insulin can be administered via injections, insulin pumps, or closed-loop pump systems with continuous glucose monitoring.
Insulin types
Since the discovery and purification of insulin in the 1920s, several insulin formulations have been developed with different pharmacodynamic properties tailored to meet patient needs throughout the day. These include rapid-acting, short-acting, intermediate-acting, and long-acting insulins.
Rapid-acting insulins like insulin lispro (Humalog), insulin aspart (Novolog), and insulin glulisine (Apidra) have the fastest onset and shortest duration of action. They are structurally modified to promote disassociation of hexamers into absorbable monomers after subcutaneous injection. Onset of action occurs within 15 min, with peak effect in 1–2 h and duration of 2–4 h. This profile mimics endogenous mealtime insulin secretion, making rapid-acting insulins ideal for prandial coverage.
Short-acting (regular) insulin reaches peak concentrations in 2–3 h and lasts for 3–6 h. While slower than rapid-acting formulations, regular insulin can also be used at mealtimes, especially when paired with longer-acting insulin. It is also used to correct hyperglycemia and in insulin infusion protocols for diabetic ketoacidosis.
Intermediate-acting insulins include neutral protamine Hagedorn (NPH) insulin which relies on protamine for delayed absorption. Its onset is around 2 h, peak effect at 4–10 h, and duration up to 18 h. NPH is an intermediate-acting insulin that has traditionally been used as basal insulin, but has been largely replaced by longer-acting analogs.
Long-acting insulin analogs more closely mimic basal insulin secretion with a flat pharmacokinetic profile. Insulin detemir (Levemir) lasts 12–24 h, and insulin glargine (Lantus) lasts up to 24 h. Insulin degludec (Tresiba) is an ultra-long-acting insulin with a half-life exceeding 24 h and duration up to 42 h, providing flexible dosing intervals.
Insulin delivery methods
The most common and longstanding method of insulin delivery is via subcutaneous injection with syringes or insulin pens. Multiple daily injection (MDI) regimens involve 2–4 injections per day of different insulin types to cover basal and prandial needs. Basal insulin is provided by long-acting insulin, while rapid-acting insulin is used for mealtime boluses. Some fixed-ratio combination products provide both basal and prandial coverage. The insulin pen devices have revolutionized MDI therapy by providing convenient, accurate insulin dosing in an easy to use design. Insulin pumps offer a continuous subcutaneous insulin infusion, with rapid-acting insulin being delivered at variable basal rates and bolus doses around meals and corrections. The pumps are programmed to meet an individual's insulin needs and can provide higher doses that mimic natural peaks. Pumps reduce hypoglycemia risk and provide lifestyle flexibility without multiple daily injections. However, they require more extensive patient education for appropriate use. Closed-loop pump systems incorporate continuous glucose monitoring with automated insulin delivery guided by sensor glucose readings. Also known as artificial pancreas systems, they represent the most physiologic insulin replacement by automatically adjusting insulin infusion based on current and predicted near-future glucose levels. Hybrid closed-loop systems still require patient meal boluses, while fully automated systems provide complete basal and bolus dosing. Clinical trials demonstrate improved glycemic control, reduced hypoglycemia, and decreased patient burden with these advanced systems (Cudini and Fierabracci 2023).
Lifestyle modifications
In addition to exogenous insulin therapy, the management of type 1 diabetes (T1D) relies heavily on lifestyle modifications to achieve optimal glucose control and prevent both acute and long-term complications. These include appropriate dietary patterns, regular exercise, weight control, frequent blood glucose monitoring, and diligent avoidance of hypoglycemia and other diabetes-related complications.
Diet and exercise
Medical nutrition therapy is a critical component of T1D treatment. The goals are to maintain healthy body weight, optimize glycemic control, achieve normal growth and development in children, and prevent cardiovascular risks. Individualized meal planning should balance carbohydrate intake with insulin therapy, limiting sugar and refined carbohydrates while ensuring adequate whole grains, fiber, fruits, and vegetables. Adequate protein intake is important for growth and weight management. Fat intake is focused on healthier unsaturated fats. Any needed vitamin/mineral supplements are recommended. Most experts advocate for a balanced, healthy diet for the whole family rather than restrictive “diabetic diets.” Regular physical activity is also encouraged, with benefits including improved insulin sensitivity, cardiovascular fitness, weight control, and mental health. At least 60 min daily of moderate aerobic and muscle-strengthening exercise is recommended for children, building up to 150 min per week for adults. Activity levels may need to be adjusted around insulin peaks and troughs to prevent hypo/hyperglycemia. Patients must monitor blood glucose before, during, and after exercise and adjust insulin or consume supplemental carbs as needed. Weight control through diet and exercise is key, as obesity worsens insulin resistance. Modest 5–10% weight loss can improve glycemic control, lipids, and blood pressure in overweight T1D patients. Growth monitoring in children ensures appropriate weight gain and growth velocity. Nutrition education and guidance around meal planning, carbohydrate counting, glycemic index, and healthy lifestyles are provided by diabetes educators and dietitians as part of comprehensive education.
Blood glucose monitoring
Frequent self-monitoring of blood glucose (SMBG) is essential for achieving glycemic targets. Testing is recommended 3 or more times daily, including both pre- and post-prandial levels to guide insulin adjustments. More frequent monitoring is appropriate with insulin pumps, exercise, hypoglycemia, illness, pregnancy, or labile glucose. Continuous glucose monitoring (CGM) provides 24/7 interstitial glucose readings displayed in real-time on receivers or phones. CGM aids early detection of hyper/hypoglycemia and trends. Combining CGM with insulin pumps enables automated insulin delivery. Patients must be proficient in interpreting and responding to glucose data.
Complication prevention
Preventing both acute (hypoglycemia, DKA) and long-term (microvascular, macrovascular) diabetes complications is imperative. Hypoglycemia can result from mismatch in insulin timing, over-correction of hyperglycemia, missed meals, exercise, alcohol use, etc. Mild hypoglycemia may be treated with oral glucose, while severe cases require glucagon injection or intravenous dextrose. Patients should carry emergency glucose sources at all times. Diabetic ketoacidosis requires emergency medical treatment with fluids, electrolyte correction, and insulin therapy. Reducing risks of microvascular and macrovascular complications long term requires diligent glucose management and control of blood pressure and lipids. Annual eye, kidney, foot and dental examinations screen for retinopathy, nephropathy, neuropathy, and vascular disease. Patient education emphasizes lifestyle habits and self-care practices that minimize risks of acute and chronic complications for optimal longevity and quality of life (Tomah et al. 2023).
Novel and emerging therapies
Pancreatic islet transplantation
Despite advances in exogenous insulin therapy and technology, type 1 diabetes (T1D) remains burdensome due to the challenges of maintaining strict glycemic control to prevent complications. This has driven research into novel therapeutic approaches beyond traditional insulin replacement, including regenerative strategies to restore endogenous insulin production. Pancreatic islet transplantation involves infusing isolated insulin-producing islets from an organ donor pancreas into the liver of a T1D patient via the portal vein. Once engrafted, the functional islet beta cells can sense blood glucose and secrete insulin, restoring glucose-responsive endogenous insulin production without the need for exogenous insulin therapy. Islet transplantation is potentially curative for T1D, but still considered an experimental procedure with limited availability. Though first attempted in the 1970s, major advances occurred in the 2000s with the Edmonton protocol which used a steroid-free immunosuppressive regimen and multiple donors per recipient. This achieved insulin independence in most recipients, proving the efficacy of islet transplantation (Addissouky et al. 2024a, 2024b).
However, long-term outcomes showed that less than 10% remained insulin-free at 5 years. Most recipients achieved excellent glycemic control and hypoglycemia prevention, despite still needing some exogenous insulin. The procedure involves isolating islets from brain-dead donor pancreata using collagenase digestion and gradient purification. The optimal source is younger donors with low body mass index and short cold ischemia time. Isolation protocols have become more efficient, with > 500,000 islet equivalents typically transplanted per patient in 2–3 infusions. Infusing islets into the hepatic portal vein enables efficient engraftment and glucose sensing. Initial immunosuppression prevents allorejection using a combination of sirolimus, tacrolimus, and/or anti-IL-2 receptor antibodies. Immunosuppression is required long term to prevent autoimmune recurrence. Limitations currently restrict islet transplantation to patients having severe glycemic lability and hypoglycemia unawareness despite optimal insulin therapy. The shortage of cadaveric pancreas donors makes wide availability challenging. Ongoing research aims to improve efficacy, durability, and applicability by exploring transplantation sites besides the liver, encapsulation devices to protect islets from immune attack, donor pig islets as an alternative tissue source, and methods to induce immune tolerance of transplanted islets (Kabakchieva et al. 2023).
Xenotransplantation
Xenotransplantation is the transplantation of cells, tissues, or organs from another species to humans. Pigs represent a potential unlimited source of insulin-producing islet cells for transplantation into T1D patients. Porcine insulin-producing cells are functionally similar to human islets but not rejected by the recipient's immune system. Preclinical research and clinical trials are investigating the efficacy, safety, and immunological issues surrounding transplantation of pig islets or pancreatic tissue. Pig islets have been transplanted into diabetic primates with successful function in normalizing blood glucose without immunosuppression (Addissouky et al. 2023c).
However, in clinical trials, pig islet transplant alone has required immunosuppression to achieve even temporary function without long-term insulin independence. Approaches to prevent immunological rejection and permit long-term graft survival are being developed, including genetic engineering of donor pigs to remove antigens that trigger human immune responses. Encapsulation devices may also protect xenografts from rejection. Additional concerns around xenotransplantation include transmission of pig endogenous retroviruses (PERVs) to humans. No cases have been documented so far, and screening methods to detect PERV infection in pigs are advancing. Ethical issues regarding appropriate animal husbandry and welfare standards must also be considered (Citro et al. 2023).
Proteomics and genomics
The pathophysiology and clinical progression of type 1 diabetes (T1D) varies greatly between individuals, driven by differences in genetics, immune phenotypes, and environmental exposures. This heterogeneity has spurred interest in precision medicine approaches that tailor prevention and treatment based on an individual's genomic and proteomic data. Leveraging proteomics and genomics may enable more personalized strategies to prevent, reverse, or appropriately manage autoimmune diabetes.
Proteomics
Proteomics involves characterization of the entire set of proteins expressed by the genome, including variations in protein abundance, structure, function, and interactions. Since proteins directly execute cellular functions, analysis of protein expression changes in T1D can reveal insights into disease pathogenesis and mechanisms. Proteomic profiling of blood or tissues can identify biosignatures that stratify risk for T1D development, detect disease early, or predict progression. This may guide individually tailored prevention, screening, and treatment approaches. Several studies have performed proteomic analysis of plasma from autoantibody positive individuals who later progressed to T1D compared to those that did not. Differentially expressed proteins related to complement activation, lipid metabolism, and cytokine signaling were able to predict T1D development. Other efforts using serum have defined protein signatures that distinguish the presence or absence of autoantibodies and progression rate to T1D. Ongoing research aims to develop blood-based protein biosignatures that enhance predictive accuracy for T1D above genetic and autoantibody testing alone. Proteomic examination of pancreas specimens has also elucidated potential tissue biomarkers of T1D. Proteins involved in regulating apoptosis and proteolysis were abnormal, implicating protease activation in pancreatic beta cell death. Analysis of pancreatic fluids and islet secretions may provide further insights into islet-specific protein changes. Integration of multiple omics datasets including genomics, transcriptomics, and metabolomics will strengthen predictive capabilities and mechanistic inferences. Ultimately, the goal is to use proteomic profiling to assign T1D subgroups for personalized management. Patients predicted to have rapidly progressing autoimmunity may benefit from more aggressive immunotherapy, while those predicted to have a slower decline could avoid overtreatment. Proteomics may also aid development of biomarker-driven therapies targeting relevant molecular pathways (Syed et al. 2023).
Genomics
Genomic analysis evaluates genetic variability to determine T1D risk, prognosis, and tailored interventions. Genome-wide association studies (GWAS) have identified over 60 genomic loci associated with T1D susceptibility. Genetic testing can identify high-risk HLA haplotypes and non-HLA variants, allowing quantification of polygenic risk scores. Patients with high genetic risk could be preferentially enrolled in prevention trials or receive counseling about risk-reducing behaviors. Genotyping key loci also enables subclassification into genetically distinct subtypes of T1D. For example, patients lacking high-risk HLA genotypes may have certain monogenic forms of diabetes that require alternative management. Analyzing autoantibody positive individuals for genetic risk scores improves prediction of T1D progression and allows appropriate targeting of secondary prevention efforts.
Pharmacogenomics assesses genetic determinants of drug response to enable individualized therapy. Genotyping cytochrome p450 enzymes, insulin analog receptors, and immune regulatory molecules may guide optimal insulin type, dosing, and possibly immunotherapy. For prevention trials, genetic screening is necessary to target subjects likely to respond and exclude non-responders. Whole genome, exome, or RNA sequencing provides comprehensive genetic data for precision medicine but is not yet practical clinically. As sequencing costs decrease and bioinformatic tools improve, analyzing complete genetic variability may become viable and enhance unraveling of genetic-environmental interactions in T1D pathogenesis. Novel immunotherapies and regenerative medicine strategies aim to preserve and replace beta cell mass in T1D. Therapeutic targets include modulating T/B cell responses, inhibiting cytokine signaling, regenerating beta cells from stem cell sources, and enabling tolerance of transplanted islets. Combinatorial approaches are needed to simultaneously block autoimmunity, replace lost cells, and support engraftment. Closed-loop pump systems represent an artificial pancreas by linking continuous glucose monitoring with automated insulin delivery adjusted by control algorithms. Fully autonomous systems determine basal needs and meal boluses without user input (Luckett et al. 2023).
Stem cell therapy
Type 1 diabetes (T1D) results from autoimmune destruction of insulin-producing pancreatic beta cells. An appealing therapeutic strategy involves regenerating new functional beta cells using stem cells to replace those lost in T1D. Stem cells are primitive cells that can self-renew and give rise to more differentiated cell types. Harnessing stem cells to regenerate beta cells could potentially cure T1D by restoring a patient's ability to produce their own insulin. Different stem cell sources and methodologies are being investigated to generate insulin-secreting beta-like cells for transplantation into T1D patients. Major approaches include embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), and adult stem/progenitor cells from sources like the pancreas, liver, adipose tissue, and bone marrow. Each have advantages and disadvantages regarding availability, capacity to proliferate, and ability to differentiate into beta cells (Işildar et al. 2022).
Embryonic stem cells
Embryonic stem cells (ESCs) are derived from the inner cell mass of blastocyst stage embryos. They are pluripotent, capable of unlimited self-renewal and differentiating into all somatic cell types. Over the past two decades, protocols have been developed to differentiate ESCs in a stepwise fashion into beta-like cells expressing insulin and other beta cell markers. However, the resulting cells are immature and lack complete functional maturity. Their utility is also limited ethically and by allogenic immune rejection risks with transplantation (Singh et al. 2023).
Induced pluripotent stem cells
Induced pluripotent stem cells (iPSCs) are generated by reprogramming adult somatic cells like skin fibroblasts back into a pluripotent state via forced expression of specific genes. Patient-derived iPSCs can differentiate into replacement beta cells that are autologous, avoiding immune rejection. Studies have demonstrated in vitro generation of glucose-responsive insulin-secreting cells from human iPSCs. Translation to clinical therapy is in early phases. Safety concerns around tumorigenicity of undifferentiated cells and optimal transplantation sites need to be addressed. Encapsulation may enable retrieval if necessary (Montanucci et al. 2023).
Pancreatic progenitors
The adult pancreas contain pancreatic progenitor cells involved in normal tissue turnover that can be expanded and differentiated into beta cells. Multipotent cells have been isolated from pancreatic ducts and islets that display some beta cell plasticity. Pancreatic tissue obtained from organ donors provides another potential source of progenitors. Isolation protocols and differentiation factors to convert progenitors into functional beta cells with adequate yield require improvement.
Other adult stem cells
Mesenchymal stem cells (MSCs) derived from bone marrow, adipose tissue, umbilical cord, and other sources have shown some ability to transdifferentiate toward a beta cell phenotype. MSCs are likely not a robust source for generation of fully functional, glucose-responsive beta cells but may have immunomodulatory effects in T1D. Liver stem cells and GI epithelium have been proposed as potential origins of insulin-expressing cells. None have conclusively demonstrated adequate beta cell neogenesis (Farid et al. 2023).
Nanomedicine
Nanomedicine utilizes engineered nanoparticles to precisely deliver therapies to target locations in the body. Applying nanotechnology to treat type 1 diabetes (T1D) involves designing nanoparticles to carry and release immunomodulatory drugs aimed at preserving insulin-producing beta cells. Nanoparticle platforms can ferry agents that modulate immune cells and cytokines to intervene in disease pathogenesis. This may enable tissue-specific therapy without systemic immunosuppression. Several properties make nanoparticles well-suited as T1D immunotherapies. Their small size facilitates movement out of circulation into tissues and enables uptake into target immune cells. A high surface area-to-volume ratio allows multifunctional modifications like tissue-specific ligands. Nanoparticles physically protect cargo drugs from degradation and inactivation. Controlled release kinetics provide sustained delivery to maintain therapeutic levels of rapidly cleared agents (Vijayakumar and Kim 2022). Examples of nanoparticle systems being explored as T1D immunotherapies include:
Polymeric nanoparticles
Polymer-based nanoparticles formulated from materials like poly-lactic-co-glycolic acid (PLGA) provide versatile drug delivery platforms. Polymeric nanoparticles can encapsulate immunomodulatory agents and release them in a controlled manner by diffusion or polymer degradation. Tuning polymer properties modulates the drug release profile. Surface functionalization with targeting moieties promotes selective tropism toward pancreatic tissues and immune cells. PLGA nanoparticles carrying rapamycin demonstrated ability to reverse hyperglycemia in mouse models by promoting regulatory T cells and inhibiting effector T cells to reestablish tolerance. PLGA nanoparticles have also enabled oral delivery of insulin peptides to stimulate systemic tolerance against beta cells. The biocompatibility and biodegradability of polymeric nanoparticles make them promising for translation to clinical applications (Valdés Álvarez and Rojas-López 2023).
Lipid-based nanocarriers
Liposomes and solid lipid nanoparticles (SLNs) composed of physiological lipids are biocompatible platforms being utilized to deliver immunosuppressive and tolerance-inducing drugs for T1D. Liposomes encapsulate agents within the aqueous core or bilayer shell, protecting them from clearance and degradation. SLNs prepared from semi-solid lipids can integrate agents within the solid matrix. Oral insulin delivery using SLNs is being investigated to induce oral tolerance to beta cells and improve glycemic control (Huang et al. 2023).
Dendrimers
Dendrimers are highly branched, well-defined polymeric nanostructures that allow precise nanoscale engineering and multivalent presentation of biological ligands. Dendrimer-based nanoparticles have been designed to target diabetogenic immune cells and deliver payloads that delete or silence autoreactive T cells and shift the balance toward regulation. Dendrimers also enable nanoparticle uptake into lymphocytes and pancreatic tissues. The well-controlled synthesis of dendrimers allows customization for targeted immunotherapy (Raghav et al. 2022).
Inorganic nanoparticles
Inorganic materials like silica nanoparticles and gold nanorods are also being engineered as therapeutic carriers. Silica nanoparticles protect encapsulated agents from deactivation and provide controlled release. They have been used to ferry antisense oligonucleotides that modify gene expression and silence pro-inflammatory cytokines in T1D models. Gold nanorods accumulate preferentially in pancreatic tissues upon infrared irradiation, allowing localized delivery when coupled to insulin peptides (Jing et al. 2022).
Artificial organs and the use of AI and machine learning
Advances in biomedical engineering and materials science have enabled development of artificial organs to replace functions lost in disease. For type 1 diabetes, artificial pancreas devices utilizing AI and machine learning algorithms replicate aspects of glucose homeostasis. These technologies aim to automate insulin delivery in a more personalized, precise manner than current methods (Addissouky et al. 2024c, 2023d).
Artificial pancreas systems
Artificial pancreas systems are comprised of three components—a continuous glucose monitor (CGM), an insulin pump, and a control algorithm that links the two by automating insulin dosing based on current glucose levels. CGMs provide real-time interstitial glucose measurements, while insulin pumps deliver rapid-acting insulin subcutaneously. Early versions used simple threshold-based algorithms, but current systems incorporate sophisticated AI algorithms to determine optimal insulin delivery (Dermawan and Purbayanto 2022).
AI-driven automated insulin delivery
Integrating AI and machine learning algorithms allows artificial pancreas systems to analyze CGM data, learn an individual’s insulin needs, and customize delivery rather than rely on fixed programmed settings. Techniques like fuzzy logic, neural networks, and predictive control modeling mimic complex clinical decision making (Addissouky et al. 2024d, 2024e).
Utilizing past trends and data patterns, AI algorithms can forecast future glucose levels and preemptively adjust insulin dosage. Some systems are hybrid closed loops, still needing user input for announcing meals and calibrating carbohydrate intake. Fully automated artificial pancreas systems using AI determine basal needs and calculate mealtime boluses autonomously. The sophisticated self-learning abilities reduce user burden for inputting data and tailor therapy based on fluctuating daily insulin demands (Cambuli and Baroni 2023).
Benefits of AI-driven systems
Clinical trials demonstrate artificial pancreas systems with AI algorithms significantly improve glycemic control, reduce hypoglycemia episodes, and ease patient burden compared to sensor-augmented pump therapy. Users had less worry about managing blood glucose fluctuations. Automating insulin delivery using patient-specific AI modeling gave tighter control than standardized formulas. The adaptive capabilities of AI systems accommodate variations in insulin sensitivity, insulin action timing, and glucose absorption that affect optimal insulin dosing. Machine learning techniques applied to large datasets also enable detection of predictive patterns that humans cannot discern to further optimize insulin delivery. As more data are aggregated, the algorithms become more personalized and precise.
Challenges and future directions
While showing great promise, barriers remain in translating fully automated AI-driven artificial pancreas systems to widespread clinical use. Most have only been tested in controlled research settings over limited timespans. Technical challenges around sensor accuracy, connectivity, and reliability need to be optimized. Safety protocols and technologies to automatically detect and mitigate failure are critical. User trust in AI-guided autonomous systems needs to be fostered, and ethical principles established regarding data privacy and algorithm transparency. Regulatory approval pathways also need to be better defined. As these devices evolve to address limitations, integrate with emerging technologies like microneedle sensors, and expand clinical learnings, AI-driven artificial pancreas systems could transform type 1 diabetes management (Andellini et al. 2023).
Herbal and traditional Chinese medicine
Plants have been used medicinally for centuries in many traditional systems like Ayurveda, traditional Chinese medicine, and Native American herbalism. Some herbs are being investigated for immunomodulating effects relevant to type 1 diabetes (T1D) pathogenesis. Certain phytochemicals appear to have anti-inflammatory, antioxidant, and cytoprotective properties that could preserve residual beta cell function (Addissouky et al. 2024f; Addissouky et al. 2024g; Addissouky et al. 2020).
However, rigorous evidence for clinical efficacy in humans is still lacking. Preclinical studies have evaluated various herbal extracts and phytocompounds that have shown protective effects in rodent and in vitro models of T1D. For example, resveratrol reduced immune cell infiltration and pro-inflammatory cytokines in the pancreatic islets of non-obese diabetic (NOD) mice. Curcumin treatment delayed diabetes onset and preserved insulin-positive cells along with anti-inflammatory effects in NOD mice. Berberine, from plants like barberry, ameliorated hyperglycemia and boosted pancreatic antioxidant defenses in diabetic rats. Other plant compounds like epigallocatechin gallate (EGCG), capsaicin, naringenin, and quercetin inhibited autoimmune cytokine production and apoptotic signaling in vitro, suggesting potential to protect beta cells from autoimmune attack (Gang et al. 2023).
The putative mechanisms underlying the anti-diabetic effects of herbs and phytochemicals are diverse. They include antioxidant activity to counter oxidative stress-induced beta cell damage; suppression of pro-inflammatory cytokines like IL-1beta, TNF-alpha; inhibition of T cell proliferation and autoimmune phenotype; upregulation of protective cytokines like IL-4; modulation of gut microbiome dysbiosis; induction of regulatory T cells; reduction in autoantibody levels; protection against apoptosis by decreasing caspase activation; promoting survival signaling proteins like AKT/PI3K; and enhancing pancreatic beta cell proliferation and regeneration (Montanucci et al. 2023). The pleiotropic effects target various arms of the autoimmune inflammatory process as well as directly promote beta cell health and survival. This multi-pronged immunomodulation could potentially prevent T1D onset or halt progression in early disease (Shamsudin et al. 2022).
Specific herbs reported to have anti-diabetic immunomodulatory activity include turmeric (Curcuma longa), ginger (Zingiber officinale), milk thistle (Silybum marianum), astragalus (Astragalus membranaceus), licorice (Glycyrrhiza glabra), bitter melon (Momordica charantia), cinnamon (Cinnamomum cassia), fenugreek (Trigonella foenum-graecum), garlic (Allium sativum), holy basil (Ocimum tenuiflorum), ginseng (Panax ginseng), resveratrol (Polygonum cuspidatum), and berberine (Berberis vulgaris). However, purity, standardization, and optimal dosing of herbal products remain a challenge. Well-designed robust clinical trials are needed to evaluate safety and efficacy in humans (Gupta et al. 2017). Moreover, the gut microbiota is altered in both type 1 diabetes (T1D) and type 2 diabetes (T2D) patients, indicating an etiological relationship between the gut microbiota and diabetes. Studies show the microbiome of T1D has reduced diversity and increased Firmicutes, while T2D patients have increased opportunistic pathogens and decreased butyrate-producers. Genera like Bifidobacterium, Bacteroides, and Faecalibacterium negatively correlate with T2D, while Ruminococcus, Fusobacterium, and Blautia positively correlate. Dysbiosis of the gut microbiota contributes greatly to the pathogenesis of diabetes (Liu et al. 2023). Few rigorous human trials have been completed, with inconsistent results to date. Small studies of berberine and curcumin suggested anti-inflammatory effects but no definitive clinical improvements. Resveratrol showed potential to preserve beta cell function in recent-onset T1D. Some trials of plant mixtures found benefits for glycemic control and antioxidant status (Jacob and Narendhirakannan 2018).
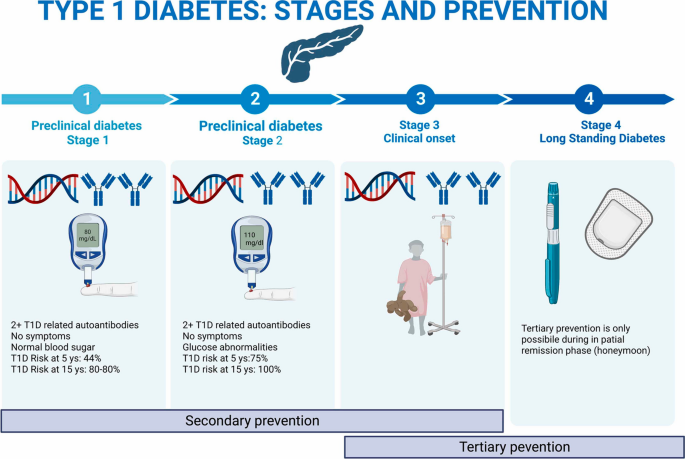
Prevention and cure
Preventing and ultimately curing type 1 diabetes (T1D) remains an elusive goal despite extensive research. Prevention encompasses primary strategies to intercept disease before onset, secondary efforts to preserve residual beta cell mass at diagnosis, and tertiary approaches to halt progression of complications. A cure likely requires regenerating functional beta cells or restoring endogenous insulin production. Combination immunotherapies, gene therapies, and regenerative medicine are being explored to reverse established T1D. Prediction involves detecting autoantibodies and genetic risk. Progression is heterogeneous but staging helps identify high-risk individuals. Prevention trials have targeted high-risk children or those with autoantibodies, using immunomodulators, antigens, or probiotics, to delay onset. Optimal timing balances early intervention against burden of diagnosis, requiring broad screening of genetic risk and autoantibodies as illustrated in Fig. 2 (Yedjou et al. 2023).
Targeted prediction and prevention strategies in T1D (Yedjou et al. 2023)
Primary prevention
Primary prevention aims to protect genetically susceptible individuals from developing autoimmune beta cell destruction. It relies on identifying risk factors and biomarkers to detect those at highest likelihood of progression. Early intervention with immunotherapy or tolerogenic vaccines that selectively target the autoreactive immune response without general immunosuppression may then prevent activation of islet autoimmunity. One approach is stimulating protective regulatory T cells using low-dose antigens like proinsulin or GAD65. Another tactic involves eliminating aggressive T cell clones and resetting immunologic balance. Ongoing trials are evaluating agents like teplizumab and abatacept that modulate T cell activation. Oral insulin to induce tolerance is also being tested. Primary prevention may be most effective during a putative “honeymoon period” before extensive beta cell loss (Mameli et al. 2023).
Secondary prevention
Secondary prevention seeks to intervene at diagnosis to salvage residual functional beta cell mass before complete destruction. Many trials have focused on immunotherapy in new-onset T1D patients to suppress inflammation and protect surviving beta cells. Drugs like anti-CD3 antibodies, CTLA-4-Ig, and IL-1 receptor antagonists showed initial disease-modifying efficacy but effects waned after treatment. Combination approaches may be required for durable effects by targeting multiple arms of autoimmunity and supporting beta cell recovery. Use of biologics, immunosuppressants, and immunoregulators needs to be balanced with potential risks. Further understanding immunopathogenic phenotypes and staging beta cell loss could personalize interventions to those with remaining targets for preservation.
Tertiary prevention
Tertiary prevention centers on halting progression of T1D complications like hypoglycemia, ketoacidosis, microvascular damage, and macrovascular disease. Diligent glucose control and self-management behaviors that minimize glycemic variability and oxidative stress are key (Addissouky et al. 2024h, 2023e). Monitoring for comorbid autoimmune conditions is also important. Optimizing glycemic control and cardiovascular risks reduces likelihood of long-term diabetes complications but cannot fully prevent them once autoimmunity is established (Francesca et al. 2023).
Cure and reversal
A complete cure likely requires reconstituting a fully functional beta cell mass capable of glucose-responsive insulin secretion after autoimmunity has developed. This remains an aspirational goal. Combination approaches to simultaneously block autoimmunity, replace beta cells, and promote survival may incrementally reverse T1D. Immune system reprogramming using gene therapies to delete or induce specific T cell populations could reset tolerance. Stem cell generation and transplantation of replacement islets offer regenerative possibilities. Xenotransplantation provides an unlimited beta cell source if hurdles are overcome. These emerging technologies suggest pathways to possible remission, if not definitive cure, are on the horizon (Weir and Bonner-Weir 2023).
Conclusions
Type 1 diabetes (T1D) remains a challenging autoimmune disorder characterized by the destruction of insulin-producing pancreatic beta cells, leading to lifelong exogenous insulin dependence and the risk of acute and chronic complications. While current management strategies involving intensive insulin therapy, lifestyle modifications, and education have improved outcomes, they do not address the underlying autoimmune pathogenesis or restore endogenous insulin production. The heterogeneity of T1D pathogenesis, driven by complex interactions between genetic susceptibility and environmental factors, highlights the need for personalized precision medicine approaches to prediction, prevention, and treatment. Elucidating individualized disease mechanisms through multi-omics technologies like proteomics and genomics holds promise for developing targeted therapies tailored to specific molecular pathways. However, the limited understanding of the precise triggers and molecular events leading to beta cell autoimmunity remains a significant limitation hindering the development of effective preventive and curative strategies.
Recommendations
To fundamentally change the trajectory of type 1 diabetes (T1D), a multifaceted approach combining innovative technologies and collaborative research efforts is recommended. Prioritizing the development of personalized precision medicine strategies, leveraging omics data and advanced bioinformatics, could enable more accurate prediction of disease risk, targeted prevention, and tailored treatment based on individual disease mechanisms. Investing in regenerative medicine approaches, such as stem cell-derived beta cell replacement therapies, xenotransplantation, and advanced encapsulation techniques, could provide a path toward restoring endogenous insulin production and potentially curing T1D. Additionally, exploring combination immunotherapies that durably modulate autoimmunity while concurrently supporting beta cell regeneration and survival could synergistically address both arms of the disease pathogenesis. Integrating these emerging therapies with cutting-edge technologies like artificial pancreas systems driven by machine learning algorithms could optimize glycemic control and reduce patient burden. Furthermore, conducting large-scale, well-designed clinical trials to rigorously evaluate the safety and efficacy of these novel interventions is crucial. Encouraging multidisciplinary collaboration among researchers, clinicians, bioengineers, and patient advocates could accelerate the translation of scientific breakthroughs into tangible therapeutic benefits for individuals living with T1D.
Availability of data and materials
All data are available, and sharing is available as well as publication.
Abbreviations
- T1D:
-
Type 1 diabetes
- DKA:
-
Diabetic ketoacidosis
- HLA:
-
Human leukocyte antigen
- GAD65:
-
Glutamic acid decarboxylase 65
- IA-2:
-
Insulinoma-associated antigen 2
- IFNγ:
-
Interferon gamma
- IL:
-
Interleukin
- TNFα:
-
Tumor necrosis factor alpha
- CGM:
-
Continuous glucose monitor
- AI:
-
Artificial intelligence
- GWAS:
-
Genome-wide association study
- iPSC:
-
Induced pluripotent stem cell
- ESC:
-
Embryonic stem cell
- MSCs:
-
Mesenchymal stem cells
- SLE:
-
Systemic lupus erythematosus
- PLGA:
-
Poly-lactic-co-glycolic acid
- SLN:
-
Solid lipid nanoparticle
- NOD:
-
Non-obese diabetic
- PERV:
-
Porcine endogenous retrovirus
References
Addissouky TA et al (2020) efficiency of mixture of olive oil and figs as an antiviral agents: a review and perspective. Int J Med Sci Health Res 4(4):107–111
Addissouky TA, Wang Y, Megahed F, El Agroudy AE, El Sayed IE, El-Torgoman AM (2021) Novel biomarkers assist in detection of liver fibrosis in HCV patients. Egypt Liver J 11(1):1–15. https://doi.org/10.1186/s43066-021-00156-x
Addissouky TA, Wang Y, El Sayed IET, El-Baz A, Ali MN, Khalil AA (2023a) Recent trends in Helicobacter pylori management: harnessing the power of AI and other advanced approaches. Beni-Suef Univ J Basic Appl Sci 12(1):80. https://doi.org/10.1186/s43088-023-00417-1
Addissouky TA, Ali MMA, El Sayed IET, Wang Y (2023b) Recent advances in diagnosing and treating helicobacter pylori through botanical extracts and advanced technologies. Arch Pharmacol Ther 5(1):53–66. https://doi.org/10.33696/Pharmacol.4.045
Addissouky TA, Ali MMA, El Sayed IET et al (2023c) Preclinical promise and clinical challenges for innovative therapies targeting liver fibrogenesis. Arch Gastroenterol Res 4(1):14–23. https://doi.org/10.33696/gastroenterology.4.044
Addissouky TA, Ali M, El Sayed IET, Wang Y (2023d) Revolutionary innovations in diabetes research: from biomarkers to genomic medicine. IJDO 15(4):228–242. https://doi.org/10.18502/ijdo.v15i4.14556
Addissouky TA, El Sayed I, Ali M et al (2023e) Molecular pathways in sepsis pathogenesis: recent advances and therapeutic avenues. J Cell Immunol. 5(6):174–183. https://doi.org/10.33696/immunology.5.183
Addissouky TA, Ali MMA, Sayed IETE et al (2024a) Emerging advanced approaches for diagnosis and inhibition of liver fibrogenesis. Egypt J Intern Med 36:19. https://doi.org/10.1186/s43162-024-00283-y
Addissouky TA, Sayed IETE, Ali MMA et al (2024b) Latest advances in hepatocellular carcinoma management and prevention through advanced technologies. Egypt Liver J 14:2. https://doi.org/10.1186/s43066-023-00306-3
Addissouky TA, El Sayed IET, Ali MMA, Alubiady MHS (2024c) Optical insights into fibrotic livers: applications of near-infrared spectroscopy and machine learning. Arch Gastroenterol Res 5(1):1–10. https://doi.org/10.33696/Gastroenterology.5.048
Addissouky TA, El Sayed I, Ali MMA, Wang Y, Khalil AA (2024d) Emerging technologies and advanced biomarkers for enhanced toxicity prediction and safety pharmacology. Adv Clin Toxicol 9(1):293. https://doi.org/10.23880/act-16000293
Addissouky TA, El Sayed IET, Ali MMA (2024e) Regenerating damaged joints: the promise of tissue engineering and nanomedicine in lupus arthritis. J Clin Orthop Trauma Care 6(2):2694–3248. https://doi.org/10.31579/2694-0248
Addissouky TA, El Sayed IET, Ali MMA, Wang Y, El Baz A, Elarabany N et al (2024f) Shaping the future of cardiac wellness: exploring revolutionary approaches in disease management and prevention. J Clin Cardiol 5(1):6–29. https://doi.org/10.33696/cardiology.5.048
Addissouky TA, Ali MMA, El Sayed IET, Wang Y, Khalil AA (2024g) Translational insights into molecular mechanisms of chemical hepatocarcinogenesis for improved human risk assessment. Adv Clin Toxicol 9(1):294. https://doi.org/10.23880/act-16000294
Addissouky TA, El Sayed IET, Ali MMA et al (2024h) Oxidative stress and inflammation: elucidating mechanisms of smoking-attributable pathology for therapeutic targeting. Bull Natl Res Cent 48:16. https://doi.org/10.1186/s42269-024-01174-6
Andellini M, Haleem MS, Angelini M, Ritrovato M, Schiaffini R, Iadanza E, Pecchia L (2023) Artificial intelligence for non-invasive glycaemic-events detection via ECG in a paediatric population: study protocol. Health Technol 13(1):145–154. https://doi.org/10.1007/s12553-022-00719-x
Arffman M, Hakkarainen P, Keskimäki I, Oksanen T, Sund R (2023) Long-term and recent trends in survival and life expectancy for people with type 1 diabetes in Finland. Diabetes Res Clin Pract 198:110580–110580. https://doi.org/10.1016/j.diabres.2023.110580
Bandarian F et al (2023) National and sub-national burden and trend of type 1 diabetes in 31 provinces of Iran, 1990–2019. Sci Rep 13(1):1–10. https://doi.org/10.1038/s41598-023-31096-8
Beran D, Højlund K, Besançon S et al (2023) A plan to improve global type 1 diabetes epidemiology data. Lancet Diabetes Endocrinol 11(3):154–155. https://doi.org/10.1016/s2213-8587(23)00029-3
Berthon W, McGurnaghan SJ, Blackbourn LAK et al (2023) Incidence of type 1 diabetes in children has fallen to pre-COVID-19 pandemic levels: a population-wide analysis from Scotland. Diabetes Care. https://doi.org/10.2337/dc23-2068
Cambuli VM, Baroni MG (2023) Intelligent insulin versus artificial intelligence for type 1 diabetes: will the real winner please stand up? Int J Mol Sci 24(17):13139–13139. https://doi.org/10.3390/ijms241713139
Citro A, Neroni A, Pignatelli C, Campo F, Policardi M, Monieri M, Pellegrini S, Dugnani E, Manenti F, Maffia M, Valla L, Kemter E, Marzinotto I, Olgasi C, Cucci A, Follenzi A, Lampasona V, Wolf E, Piemonti L (2023) Directed self-assembly of a xenogeneic vascularized endocrine pancreas for type 1 diabetes. Nat Commun 14(1):878. https://doi.org/10.1038/s41467-023-36582-1
Corsello A, Immacolata C, Milani GP, Agostoni C (2023) Vitamin D in pediatric age: current evidence, recommendations, and misunderstandings. Front Med 10:1107855. https://doi.org/10.3389/fmed.2023.1107855
Cudini A, Fierabracci A (2023) Advances in immunotherapeutic approaches to type 1 diabetes. Int J Mol Sci 24(11):9220. https://doi.org/10.3390/ijms24119220
Dermawan D, Purbayanto MA (2022) An overview of advancements in closed-loop artificial pancreas system. Heliyon 8(11):e11648–e11648. https://doi.org/10.1016/j.heliyon.2022.e11648
Dinić S, Jovanovic J, Uskoković A, Mihailović M, Grdović N, Tolić A, Rajić J, Đorđević M, Vidaković M (2022) Oxidative stress-mediated beta cell death and dysfunction as a target for diabetes management. Front Endocrinol 2022:13. https://doi.org/10.3389/fendo.2022.1006376
Farid A, El-Alfy L, Madbouly N (2023) Bone Marrow-derived mesenchymal stem cells transplantation downregulates pancreatic NF-ΚB and pro-inflammatory cytokine profile in rats with type I and type II-induced diabetes: a comparison study. Biologia. https://doi.org/10.1007/s11756-023-01436-0
Francesca M, Primavera M, Samvelyan S, Tagi VM, Chiarelli F (2022) Stress and diabetes mellitus: pathogenetic mechanisms and clinical outcome. Hormone Res Paediatr 96(1):34–43. https://doi.org/10.1159/000522431
Francesca M, Quarta M, Quarta A, Chiarelli F (2023) Prevention of type 1 diabetes in children: A worthy challenge? Int J Environ Res Public Health 20(11):5962–5962. https://doi.org/10.3390/ijerph20115962
Gang R, Matsabisa MG, Okello D, Kang YM (2023) Ethnomedicine and ethnopharmacology of medicinal plants used in the treatment of diabetes mellitus in Uganda. Appl Biol Chem 66(1):39. https://doi.org/10.1186/s13765-023-00797-z
Gupta RC, Chang DH-T, Nammi S, Bensoussan A, Bilinski K, Roufogalis BD (2017) Interactions between antidiabetic drugs and herbs: an overview of mechanisms of action and clinical implications. Diabetol Metab Syndr. https://doi.org/10.1186/s13098-017-0254-9
Holborough-Kerkvliet MD, Kroos S, van de Wetering R, Toes REM (2023) Addressing the key issue: antigen-specific targeting of B cells in autoimmune diseases. Immunol Lett 259:37–45. https://doi.org/10.1016/j.imlet.2023.05.005
Hormazábal-Aguayo I, Ezzatvar Y, Huerta-Uribe N, Ramírez-Vélez R, Izquierdo M, García-Hermoso A (2024) Incidence of type 1 diabetes mellitus in children and adolescents under 20 years of age across 55 countries from 2000 to 2022: a systematic review with meta-analysis. Diabetes Metab Res Rev 40(3):e3749. https://doi.org/10.1002/dmrr.3749
Huang M, Chen W, Wei M, Huang Y, Liu H, Yue M, Chen Y, Tang Z, Jia B (2023) Advanced delivery strategies for immunotherapy in type I diabetes mellitus. BioDrugs 37(3):331–352. https://doi.org/10.1007/s40259-023-00594-6
Işildar B, Özkan S, Ercin M, Gezginci-Oktayoglu S, Öncül M, Koyutürk M (2022) 2D and 3D cultured human umbilical cord-derived mesenchymal stem cell-conditioned medium has a dual effect in type 1 diabetes model in rats: immunomodulation and beta-cell regeneration. Inflamm Regen 42(1):55. https://doi.org/10.1186/s41232-022-00241-7
Jacob B, Narendhirakannan RT (2018) Role of medicinal plants in the management of diabetes mellitus: a review. 3 Biotech. https://doi.org/10.1007/s13205-018-1528-0
Jing Z, Li Y, Ma Y, Zhang X, Liang X, Zhang X (2022) Leverage biomaterials to modulate immunity for type 1 diabetes. Front Immunol 13:997287. https://doi.org/10.3389/fimmu.2022.997287
Kabakchieva P, Assyov Y, Gerasoudis S, Vasilev G, Peshevska-Sekulovska M, Sekulovski M, Lazova S, Miteva D, Gulinac M, Tomov L, Velikova T (2023) Islet transplantation-immunological challenges and current perspectives. World J Transpl 13(4):107–121. https://doi.org/10.5500/wjt.v13.i4.107
Liu Y, Deng S, Song Z, Zhang Q, Guo Y, Yu Y, Wang Y, Li T, Megahed F, Addissouky TA, Mao J, Zhang Y (2021) MLIF modulates microglia polarization in ischemic stroke by targeting EEF1A1. Front Pharmacol 12:725268. https://doi.org/10.3389/fphar.2021.725268
Liu B, Zhang L, Yang H, Wang C-Y, Liao X (2023) Microbiota: a potential orchestrator of antidiabetic therapy. Front Endocrinol 14:973624. https://doi.org/10.3389/fendo.2023.973624
Luckett AM, Weedon MN, Hawkes G, Leslie RD, Oram RA, Grant SFA (2023) Utility of genetic risk scores in type 1 diabetes. Diabetologia 66(9):1589–1600. https://doi.org/10.1007/s00125-023-05955-y
Mameli C, Triolo TM, Chiarelli F, Rewers M, Zuccotti GV, Simmons KM (2023) Lessons and gaps in the prediction and prevention of type 1 diabetes. Pharmacol Res 193:106792–106792. https://doi.org/10.1016/j.phrs.2023.106792
Montanucci P, Pescara T, Greco A, Basta G, Calafiore R (2023) Human induced pluripotent stem cells (HiPSC), Enveloped in elastin-like recombinamers for cell therapy of type 1 diabetes mellitus (T1D): preliminary data. Front Bioeng Biotechnol. https://doi.org/10.3389/fbioe.2023.1046206
Murdaca G, Paladin F, Borro M, Ricciardi L, Gangemi S (2023) Prevalence of autoimmune and autoinflammatory diseases in chronic urticaria: pathogenetic, diagnostic and therapeutic implications. Biomedicines 11(2):410–410. https://doi.org/10.3390/biomedicines11020410
Ogle GD, Gregory GA, Wang F, Robinson TI, Maniam J, Magliano DJ, Orchard TJ (2023) The T1D index: implications of initial results, data limitations, and future development. Curr DiabRep 23(10):277–291. https://doi.org/10.1007/s11892-023-01520-4
Ogrotis I, Koufakis T, Kotsa K (2023) Changes in the global epidemiology of type 1 diabetes in an evolving landscape of environmental factors: causes, challenges, and opportunities. Medicina. https://doi.org/10.3390/medicina59040668
Ogrotis I, Koufakis T, Kotsa K (2023) Changes in the global epidemiology of type 1 diabetes in an evolving landscape of environmental factors: causes, challenges, and opportunities. Medicina-Lithuania 59(4):668–668. https://doi.org/10.3390/medicina59040668
Popoviciu MS, Kaka N, Sethi Y, Patel N, Chopra H, Cavalu S (2023) Type 1 diabetes mellitus and autoimmune diseases: a critical review of the association and the application of personalized medicine. J Personal Med 13(3):422–422. https://doi.org/10.3390/jpm13030422
Raghav A, Ashraf H, Jeong G-B (2022) Engineered extracellular vesicles in treatment of type 1 diabetes mellitus: a prospective review. Biomedicines 10(12):3042–3042. https://doi.org/10.3390/biomedicines10123042
Rathod S (2022) Novel Insights into the immunotherapy-based treatment strategy for autoimmune type 1 diabetes. Diabetology 3(1):79–96. https://doi.org/10.3390/diabetology3010007
Shamsudin NF, Ahmed QU, Mahmood S, Shah A, Sarian MN, Khan A, Khatib A, Sabere ASM, Yusoff YM, Latip J (2022) Flavonoids as antidiabetic and anti-inflammatory agents: a review on structural activity relationship-based studies and meta-analysis. Int J Mol Sci 23(20):12605–12605. https://doi.org/10.3390/ijms232012605
Singh AK, Noor A, Singh A, Singh S, Yadav S, Kumar M, Sarma DK, Verma V (2023) Recent trends and advances in type 1 diabetes therapeutics: a comprehensive review. Eur J Cell Biol 102(2):151329–151329. https://doi.org/10.1016/j.ejcb.2023.151329
Sun F, Yang C, Wang F-X, Rong S-JM, Luo J, Lu W-Y, Yue T-T, Wang CY, Liu S (2023) Pancreatic draining lymph nodes (PLNs) serve as a pathogenic hub contributing to the development of type 1 diabetes. Cell Biosci 13(1):156. https://doi.org/10.1186/s13578-023-01110-7
Syed F, Singhal D, Raedschelders K, Krishnan P, Bone RN, McLaughlin M, Van JE, Mirmira RG, Yang M-L, Mamula MJ, Wu H, Liu X, Evans-Molina C (2023) A Discovery-based proteomics approach identifies protein disulphide isomerase (PDIA1) as a biomarker of β cell stress in type 1 diabetes. EBioMedicine 87:104379–104379. https://doi.org/10.1016/j.ebiom.2022.104379
Thompson PJ, Pipella J, Rutter GA, Gaisano HY, Santamaria P (2023) Islet autoimmunity in human type 1 diabetes: initiation and progression from the perspective of the beta cell. Diabetologia. https://doi.org/10.1007/s00125-023-05970-z
Tomah S, Salah T, Al-Badri M, Dhaver S, Gardner H, Tasabehji MW, Hamdy O (2023) Multidisciplinary intensive lifestyle intervention improves markers of nonalcoholic fatty liver disease (NAFLD) in patients with type 1 diabetes and obesity: a retrospective matched-cohort study. Clin Diabetes Endocrinol 9(1):3. https://doi.org/10.1186/s40842-023-00150-9
Valdés Álvarez K, Rojas-López M (2023) Nanoparticles targeting monocytes and macrophages as diagnostic and therapeutic tools for autoimmune diseases. Heliyon 9(9):e19861–e19861. https://doi.org/10.1016/j.heliyon.2023.e19861
Vijayakumar N, Kim S (2022) The trend of organic based nanoparticles in the treatment of diabetes and its perspectives. Biomol Ther 31(1):16–26. https://doi.org/10.4062/biomolther.2022.080
Weir GC, Bonner-Weir S (2023) Induction of remission in diabetes by lowering blood glucose. Front Endocrinol 14:1213954. https://doi.org/10.3389/fendo.2023.1213954
Yedjou CG, Grigsby J, Mbemi A, Nelson D, Mildort B, Latinwo LM, Tchounwou PB (2023) The management of diabetes mellitus using medicinal plants and vitamins. Int J Mol Sci 24(10):9085–9085. https://doi.org/10.3390/ijms24109085
Acknowledgements
Authors thank all the researchers who have done great efforts on their studies. Moreover, we are grateful to the editors, reviewers, and reader of this journal.
Funding
Corresponding author supplied all study materials. There was no further funding for this study.
Author information
Authors and Affiliations
Contributions
The authors completed the study protocol and were the primary organizers of data collection, as well as the draft and revision process of the manuscript. Tamer A. Addissouky wrote the article and ensured its accuracy. All authors contributed to the discussion, assisted in designing the study and protocol, and engaged in critical discussions of the draft manuscript. Lastly, the authors (TA, MA, IE, YW) reviewed and confirmed the final version of the manuscript. Furthermore, all authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors hereby declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Addissouky, T.A., Ali, M.M.A., El Sayed, I.E.T. et al. Type 1 diabetes mellitus: retrospect and prospect. Bull Natl Res Cent 48, 42 (2024). https://doi.org/10.1186/s42269-024-01197-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-024-01197-z