- Case Report
- Open access
- Published:
The wandering spleen: case report of laparoscopic splenectomy in a pregnant woman
Bulletin of the National Research Centre volume 46, Article number: 273 (2022)
Abstract
Background
Wandering spleen is a rare condition, which is characterized by augmented mobility of the spleen, due to congenital or acquired causes. It is more frequent in multiparous women, but only a few cases are reported during pregnancy. Wandering spleen is usually asymptomatic until the onset of its possible complications, and this can mislead clinicians in reaching the correct diagnosis.
Case presentation
We report the case of a wandering spleen with acute splenic infarction in a pregnant woman and its minimally invasive surgical treatment, focusing on the clinical and radiological findings that could mislead or drive clinicians to the right diagnosis, or a potential disaster.
Conclusions
Splenic preservation in the wandering spleen where it is safe and possible is the main goal of the treatment. Clinical and radiological findings are the most relevant elements to drive surgical treatment. To reach the best and opportune treatment for the patient, the wandering spleen is an insidious condition and must be included in the differential diagnosis in the acute abdomen diagnostic process.
Background
Wandering spleen (WS) is a rare and still relatively unknown condition. It is characterized by augmented mobility of the spleen, due to a congenital lack of splenic ligaments or an acquired increased laxity of these structures.
This relaxation of the tissues may lead to spontaneous torsions of the splenic hilum, with possible subsequent acute or chronic ischemic infarctions of the spleen, making WS a deceptive and misleading condition.
Until 2012 WS cases reported in the medical literature were about 500 worldwide, almost a 0.5% of splenectomies performed (Puranik et al. 2017). Since 2012, there have been reported in the literature almost 150 new cases.
The real incidence of this pathology is surely underestimated because of the healthy carriers, making WS a silent condition until the appearance of its complications, which could also be life-threatening.
Most of the cases are reported in childbearing-age women, in particular multiparous ones. It is probably related lo the augmented laxity of the tissue due to hormonal values acquired during pregnancies.
This hypothesis is confirmed by the observation of an asymmetrical distribution of WS in the adult population between females and males, with a proportion of approximately 7:1 (Wang et al. 2020).
The second peak incidence is in the pediatric population, with equal distribution between males and females, and a medium age of fewer than 10 years old (Wang et al. 2020; Antona et al. 2022). In these cases, the WS is probably related to a congenital lack of splenic ligaments, giving the organ augmented mobility and subsequent possible acute and/or chronic torsion on its longitudinal axis.
WS rests usually unknown until the appearance of a complication, such as chronic or acute ischemic damage, resulting from the torsion of the vascular axis, leading to potentially life-threatening conditions (Sentürk et al. 2022).
For this reason, there are no clear clinical features related to WS, because it depends on the phases of the splenic wandering and could remain undiagnosed all lifelong.
In the medical literature, there are only a few cases of WS during pregnancy (Parvaiz et al. 2004; Yücel et al. 2012), getting to complex and dangerous clinical pictures, complicated by the coexistence of the fetus.
A similar diagnosis later than our case report in pregnancy (e.g., last trimester) has not occurred yet as far as we know; it could potentially become delicate and dangerous to manage and must hold into consideration the WS vascular state, and the feasibility of an urgent surgical approach. Limitations of this paper are strongly linked to the case report essence, describing a single pathological situation, that is not necessarily applicable to different clinical circumstances.
This study is a case report regarding WS and a case report of the most advanced gestational age WS during pregnancy, as far as we know in the medical literature.
This case report has been reported in line with the SCARE criteria (Agha et al. 2020).
Case presentation
LZ, is a 31-year-old Caucasian white woman, normal weight (BMI 20 kg/m2), primigravida, with no pathological history, pharmacologic chronic therapy, or allergies reported.
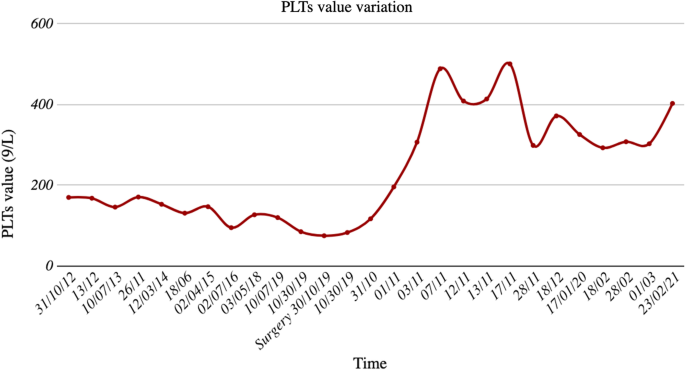
Mild thrombocytopenia was found in previous blood examinations, with a minimum value of 959 platelets/L in 2016, never examined with second-level examinations.
During the first obstetrical ultrasound check, a vascularized and capsulated mobile mass in the abdomen was detected, with a major axis of 12.5 cm, characterized by a hypertrophic and elongated hilar vascular axis. In parallel, there was no spleen in the left hypochondrium, confirming the WS diagnosis.
The WS had some parenchymal calcific strias, per previous parcellar ischemic infarctions.
This condition was asymptomatic, and the physical examination was negative for any pathological finding, with no palpable masses, and no abdominal evocable pain.
The result of the multidisciplinary consult executed was an indication of the close monitoring of WS through frequent ultrasound examinations and blood examinations, with conservative treatment because of the initial weeks of the pregnancy.
During week 17th of the pregnancy, the patient had blood examinations, demonstrating a reduction of platelets (PLTs) count to 879/L, with the stability of the WS in ultrasound check.
MRI has been planned to have more precise information and set the best treatment for the patient. During the waiting days for the scheduled MRI, on October 30, 2019, in course of the 22nd week of pregnancy, the patient got to the ER because of the onset of intense and diffuse abdominal pain during the night, without fever or any other clinical manifestation. Clinical examination confirmed the relevant widespread abdominal pain, Blumberg sign absent.
Blood examinations performed in the ER were in the range of normality, except for further thrombocytopenia, with a PLTs count of 749/L.
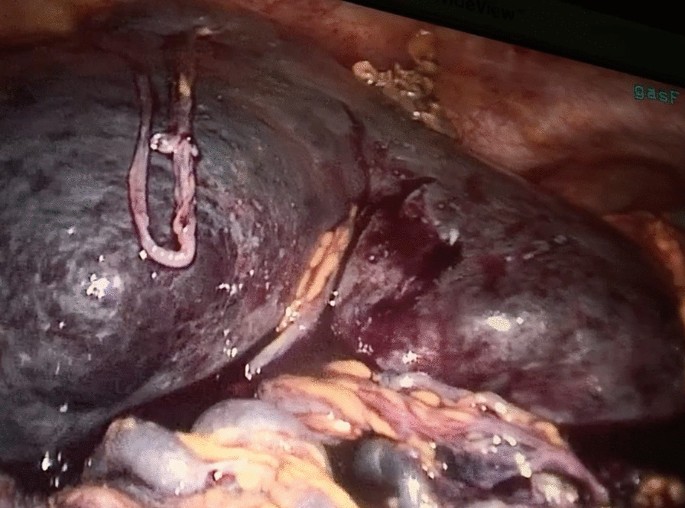
An urgent ultrasound examination was performed, observing the augmented volume of the WS (diameter 18 × 8 cm) and parenchymal ischemic injury; no vascular signal was detected at the splenic hilum with color Doppler technique, without free fluid in the belly (Fig. 1).
For this reason, the patient underwent an urgent surgical procedure.
A laparoscopic approach was decided, noticing a hypertrophic mobile spleen in subhepatic space, surrounded by a multitude of ectasic and congested vessels. The principal vascular axis of the WS was also hypertrophic, with a diameter of around 4 cm (Fig. 2).
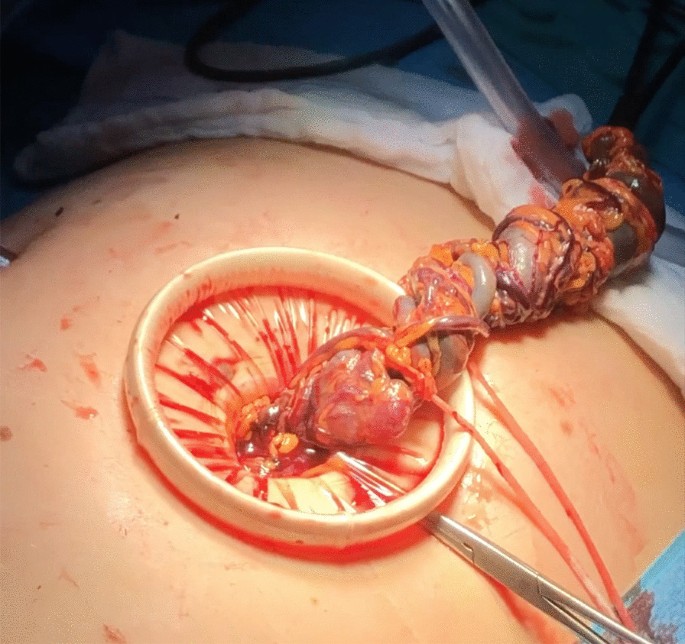
After initial mobilization of the WS, partial dissection of the perisplenic vessels, and isolation of the principal vascular axis, a median mini-laparotomy was performed to dissect and tie the hypertrophic splenic vessels with non-resorbable suture (Fig. 3).
Using laparoscopy, a complete mobilization of the WS was performed from its remaining ligaments.
Subsequent extraction of the spleen from the laparotomy was executed from the service laparotomy. Fetal parameters resulted in physiological and unaltered after surgery.
The postoperative course was regular and the PLTs count normalized in a few weeks, with a median of 3009/L. Subsequent blood examinations confirmed the normalization of PLTs values (Fig. 4).
The patient had natural childbirth at week 39th with no complications.
The patient, two weeks after delivery, received Streptococcus Pneumoniae, Haemophilus Influenzae, and Neisseria Meningitidis vaccinations, as standard prevention for most frequent severe infections after splenectomy.
Conclusions
WS is a rare and insidious condition, with many different possible manifestations, from asymptomatic patients to urgent and emergencies, requiring prompt and opportune diagnosis and treatment, making this condition very challenging for clinicians.
This case report describes a borderline case within a rare pathological entity, with pregnancy as an element of high risk.
WS is a diagnosis that must be included in the differential diagnosis in particular cases, such as multiparous women with an abdominal palpable mass or recurrent and vague abdominal pain.
The increase in WS diagnosis is supported by a constant and rapid improvement in radiological technique, getting more easily and accurately diagnosed in elective and acute examinations, making WS a less misdiagnosed life-threatening pathological entity, not only in multiparous women.
WS knowledge is principally based on an increasing number of single case reports, such as this one, driving clinicians to manage this rare and complex diagnosis, both in emergency and elective surgery.
A better understanding of WS etiopathogenesis is important to reach a complete comprehension of its pathological mechanisms, to get a better diagnostic and therapeutic ability, and to prevent a possible life-threatening condition.
Further studies are necessary to obtain a full understanding of WS’s genesis, to get a unique and standard diagnostic and therapeutic guidelines, making WS the best-known and less dangerous condition.
Availability of data and materials
All the data and images are originals and disposable upon request to the corresponding author.
Abbreviations
- WS:
-
Wandering spleen
- BMI:
-
Body mass index
- PLTS:
-
Platelets
- ER:
-
Emergency room
References
Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, SCARE Group (2020) The SCARE 2020 Guideline: updating consensus surgical CAse report (SCARE) guidelines. Int J Surg 84:226–230. https://doi.org/10.1016/j.ijsu.2020.10.034
Antona G, Arredondo Montero J, Ros Briones R, Bronte Anaut M, Moreno Ibérico MA, Bardají Pascual C (2022) Pediatric splenic torsion in an orthotopic spleen without fixation elements. J Pediatr S0022–3476(22):00730–00732. https://doi.org/10.1016/j.jpeds.2022.08.021
Parvaiz A, Chandran S, Karim A, Kumar K, Jeffrey P, Lagattolla NR (2004) Torted and ruptured wandering spleen presenting as a surgical emergency in pregnancy. Sci World J 4:1035–1037. https://doi.org/10.1100/tsw.2004.208
Puranik AK, Mehra R, Chauhan S, Pandey R (2017) Wandering spleen: a surgical enigma. Gastroenterol Report 5(3):241–243. https://doi.org/10.1093/gastro/gov034
Sentürk M, Kasikci YS (2022) Wandering spleen, which is torsioned with the distal pancreas. Distal pankreas ile birlikte torsiyone olan gezici dalak. Turk J Trauma Emerg Surg 28(9):1363–1365. https://doi.org/10.14744/tjtes.2021.34288
Wang Z, Zhao Q, Huang Y, Mo Z, Tian Z, Yang F, Wang Y, Yao L (2020) Wandering spleen with splenic torsion in a toddler: a case report and literature review. Medicine 99(37):e22063. https://doi.org/10.1097/MD.0000000000022063
Yücel E, Kurt Y, Ozdemir Y, Gun I, Yildiz M (2012) Laparoscopic splenectomy for the treatment of wandering spleen in a pregnant woman: a case report. Surg Laparosc Endosc Percutaneous Tech 22(2):e102–e104. https://doi.org/10.1097/SLE.0b013e318246beb5
Acknowledgements
Not applicable.
Funding
The authors received no financial support for this article's research, authorship, and/or publication.
Author information
Authors and Affiliations
Contributions
LC and ADL wrote the manuscript. LC, GB, and PP took part in the surgical procedure described in the present paper. LC and MG managed preoperative and postoperative indications. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical approval statement was required for this study. Fully informed written consent was obtained for surgery.
Consent for publication
Informed consent was obtained for publication.
Competing interests
The authors certify that they have no affiliations with or involvement in any organization with any financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Crepaz, L., Di Leo, A., Borzellino, G. et al. The wandering spleen: case report of laparoscopic splenectomy in a pregnant woman. Bull Natl Res Cent 46, 273 (2022). https://doi.org/10.1186/s42269-022-00960-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-022-00960-4